 |
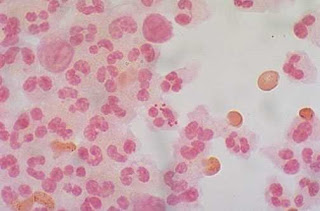
| Figure 1: Neisseria meningitidis, often referred to as meningococcus |
Diagnosis of meningitis in adults: Sensitivity of physical exam
Meningitis is a difficult-to-diagnose disease with potentially devastating consequences. Meningitis refers to inflammation (usually infectious) of the meninges, a layer of membranes that enclose the brain and spinal cord. Meningitis can be caused by bacteria, viruses, and fungi. Common causes of bacterial meningitis include Strep pneumoniae (most common bacterial cause), Hemophilus influenza, Staphylococcus aureus, Neisseria meningitidis, and Mycobacterium tuberculosis. Meningitis typically results from hematogenous spread of bacteria to seed the meninges. However, it can also occur from direct extension from sinusitis or otitis media, following neurosurgery, skull fracture, or other trauma which create a portal of entry of organisms. Without treatment bacterial meningitis is usually fatal, and even with treatment, the mortality rate is 25%.
Other causes of meningitis include viral (enterovirus, HSV), fungal (cryptococcus), and parasitic. Aspetic meningitis refers to a category in which meningeal inflammation is present but no infectious organism is identified. Most of these cases are likely viral, but partially treated bacterial meningitis can also masquerade as aseptic meningitis.
Because of its nonspecific signs and symptoms, meningitis is a notoriously difficult disease to diagnose. Physical exam findings such as Kernig's signs, Brudzinski's signs, and nuchal rigidity can aid in the diagnosis, but lack sensitivity and specificity.
A 2002 study in Clinical Infectious Disease evaluated the sensitivity of these bedside tests. 297 patients with suspected meningitis were examined prior to undergoing lumbar puncture to evaluate for meningitis (defined as >6 WBCs/mL spinal fluid). The researchers found that the sensitivities for Kernig's sign, Brudzinski's sign, and nuchal rigidity for meningitis were a dismal 5%, 5%, and 30%, respectively. In the very small subset of patients with severe meningeal irritation (4 patients; defined as >1000 WBCs/mL spinal fluid), only nuchal rigidity, but not the other two signs, had diagnostic value with a sensitivity of 100%. The conclusion of the study was that these bedside tests are "too insensitive to identify the majority of patients with meningitis in contemporary practice."
Why am I writing this post? Because I recently had a patient with fever and a headache. She had no neck stiffness and no nuchal rigidity on exam. In my mind this put the diagnosis of meningitis lower on the differential, which led to a delay in her getting a lumbar puncture, which, as it turns out, showed she did in fact have meningitis. Fortunately the the patient did well. But it was an important learning case for me. If the sensitivity of nuchal rigidity is only 30% as this study reports (similar data seen in other studies), clearly I should not have felt reassured by her lack of nuchal rigidity, any more than I would have determined that a patient with a negative psoas sign could not have appendicitis.
No single physical exam finding or historical feature can rule in, or rule out, the diagnosis of meningitis. The gold standard for diagnosis, a lumbar puncture, is a test with costs both to patient and physician, and not every patient with fever and headache should get a lumbar puncture. This would expose patients to unnecessary risks and discomfort and create a disaster of work flow in a busy ED. Rather the entire picture needs to be taken into account to push one to do the lumbar puncture: historical features, patient appearance and physical exam findings, input from family/friends, and ultimately physician "gestalt." This is what makes our job as emergency physicians challenging, and yet fun. There are no algorithms or easy formulas to apply to evasive diagnoses like meningitis. Knowing what to do when is the part of the art of medicine, something we all are all perfecting in our practice.
References:
1. Razonable, R, Cunha B. Meningitis. Available at http://emedicine.medscape.com/article/232915-overview. Accessed January 5, 2012.
2. Thomas KE, Hasbun R, Jekel J, ad Quagliarella VJ. The diagnositc accuracy of Kernig’s sign, Brudzinski’s sign, and nuchal rigidity in adults with suspected meningitis. Clin Infect Dis 2002. 35:46-52.

ReplyDeleteAm leona knight
Thanks to God and also to dr akhigbe , the great herbal man that cured me of HERPES. I contacted the virus from my partner 4 year ago, i almost spent all i had because i was restless , until i saw peoples testimony about Dr akhigbe recommendation online for how he has being curing HERPES with his herbs herbal medicine , and i emailed him and tell him my problem and he prepare my cure and send it to me through UPS and gave me instructions on how to use the herbs herbal medicine, i followed as i was instructed for 2weeks and behold after i finish drinking it i notice something in me, i went to the hospital for checkup and the result was negative and the virus was completely gone from my body. You can contact Dr akhihgb to get your herbs too and cure yourself from these virus. You can email him on DRREALAHKIGBE@GMAIL.COM or you call him and whatsapp him on +2348142454860. . Dr akhibge cure so many different type of diseases with his herbal herbs such as HERPES, HIV/AIDS. CANCER of all kind, DIABETES and so many more. I want to thank God for using Dr akhibge to cure me. He is real.